In our ongoing efforts to understand and address prejudices and how this affects society, we recently had the privilege of hosting a guest lecture by renowned psychologist and researcher, Dr. John F. Dovidio. His talk shed light on the topic of racial disparities in healthcare among minority populations in the United States, particularly in the realms of physical and mental healthcare. In this blog post, we will summarize some of the key points discussed during his lecture and delve into the social psychology behind these racial disparities in healthcare.
By Aisha Vogel (intern)
Racial Disparities in Healthcare: Understanding the Social Psychology of Prejudice
“Today in the United States there are substantial inequalities in the treatment of patients based on their race and ethnicities”, Dr. Dovidio opened his lecture on racial disparities in healthcare. He hereby refers besides others to research by Hahm et al. (2015) which revealed that Black, Latin, and Asian clients are less likely than White clients to have their depression detected or diagnosed. Furthermore, Alegria et al. (2008) found that Black and Latinx clients are significantly less likely than White clients to receive minimally adequate care, even when accounting for diagnostic differences.
To comprehend the reasons behind these racial disparities in healthcare, Dr. Dovidio explored the social psychology of prejudice. He emphasized that prejudice is not limited to a few “bad apples”, but rather stems from normal cognitive, motivational, and sociocultural processes.
One of the key factors contributing to prejudice is social categorization, which is described as a natural tendency to simplify the world and classify people (Tajfel & Turner, 1986). In the United States and other countries, race, gender, and age are primary dimensions of categorization, leading to stereotypes and biases. Dr. Dovidio highlighted that categorizing individuals into ingroups and outgroups is a universal phenomenon that can lead to various forms of discrimination, such as ageism, sexism, and racism.
From Explicit to Implicit Attitudes
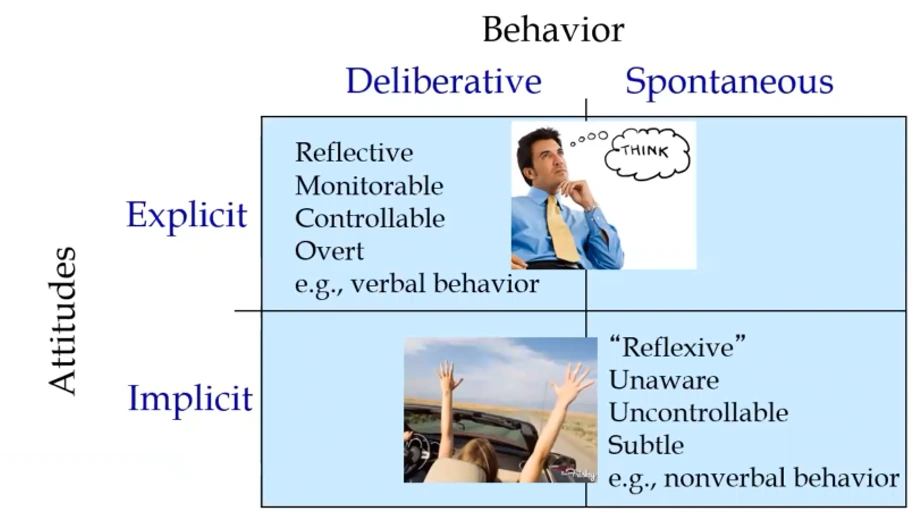
Moreover, Dr. Dovidio discussed the distinction between explicit and implicit attitudes and their role in shaping behavior. Explicit attitudes are conscious and deliberative, representing what individuals consciously report about their beliefs and values. On the other hand, implicit attitudes are unconscious, spontaneous, and reflexive. These attitudes operate automatically and can influence behavior, especially in quick and reflexive situations or when individuals are unaware of their biases.
The Nature of Racial Bias
The lecture further explored the nature of racial bias, distinguishing between explicit and implicit biases. Dr. Dovidio explained that explicit biases are the ones individuals consciously report, whereas implicit biases are automatic and often influence behavior unconsciously. Both explicit and implicit biases can coexist within an individual, with implicit biases playing a significant role in quick, reflexive behaviors and nonverbal interactions and decisions, which is discussed in the following paragraph.
Personnel Decisions and Intergroup Interactions
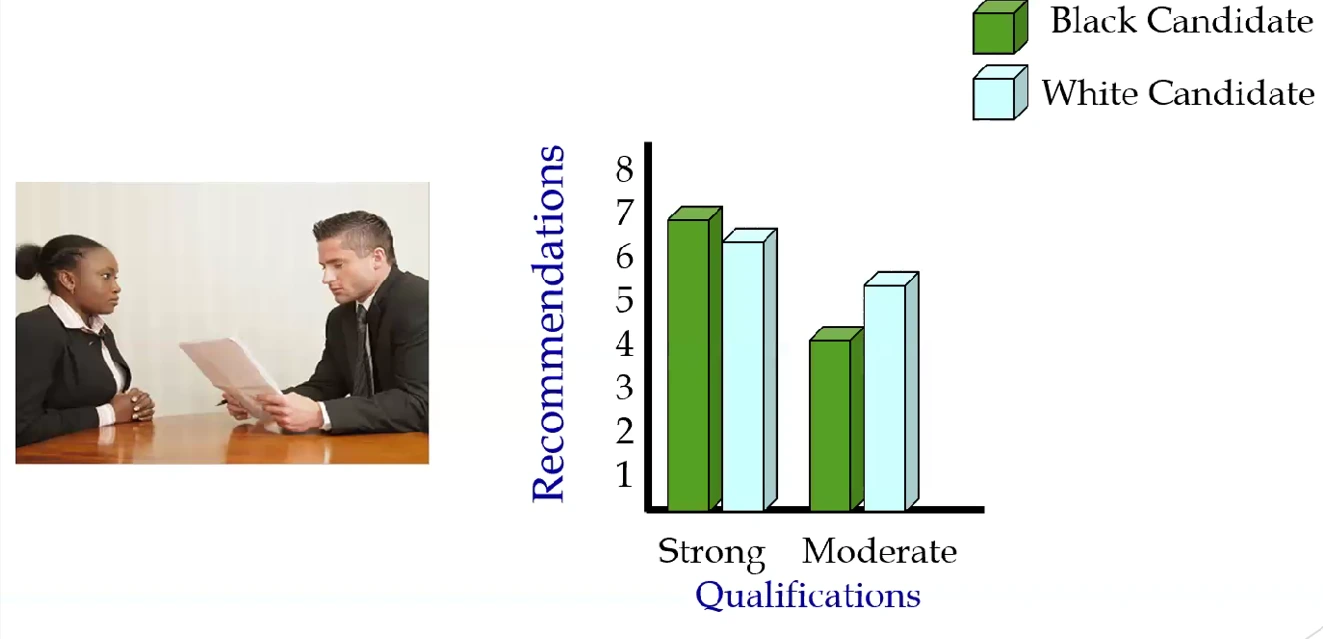
The impact of implicit biases on personal decisions was demonstrated through a study conducted by Dr. Dovidio and his colleagues. The research revealed that when evaluating job candidates with mixed qualifications, decision-makers tended to focus on the strengths of White applicants and the weaknesses of Black applicants, leading to biased decision-making. This bias, which disadvantages Black applicants, occurred even when decision-makers denied any explicit prejudice.
Dr. Dovidio also highlighted a study that examined intergroup interactions between White and Black participants. The study found that explicit attitudes predicted verbal behavior, while implicit biases affected nonverbal behavior. The Black participants, perceiving the nonverbal behavior, viewed the interactions less favorably, considering the White participants to be unfriendly and untrustworthy. This disconnect between explicit and implicit attitudes showcased the impact of implicit biases on real-life interactions. These inequalities due to biases underline the relevance of research examining such biases in everyday life, e.g. in medical and therapeutic settings. Studies examining this topic will be presented in the following.
Unveiling Implicit Bias in Medical and Therapeutic Settings
Examining the presence of implicit bias among healthcare providers is crucial to understanding how it affects patient care. Research has shown that medical professionals, including doctors, psychologists, and counselors, exhibit implicit bias, similar to the general population (Green et al., 2023). These biases can potentially influence treatment decisions and patient interactions, leading to racial disparities in healthcare.
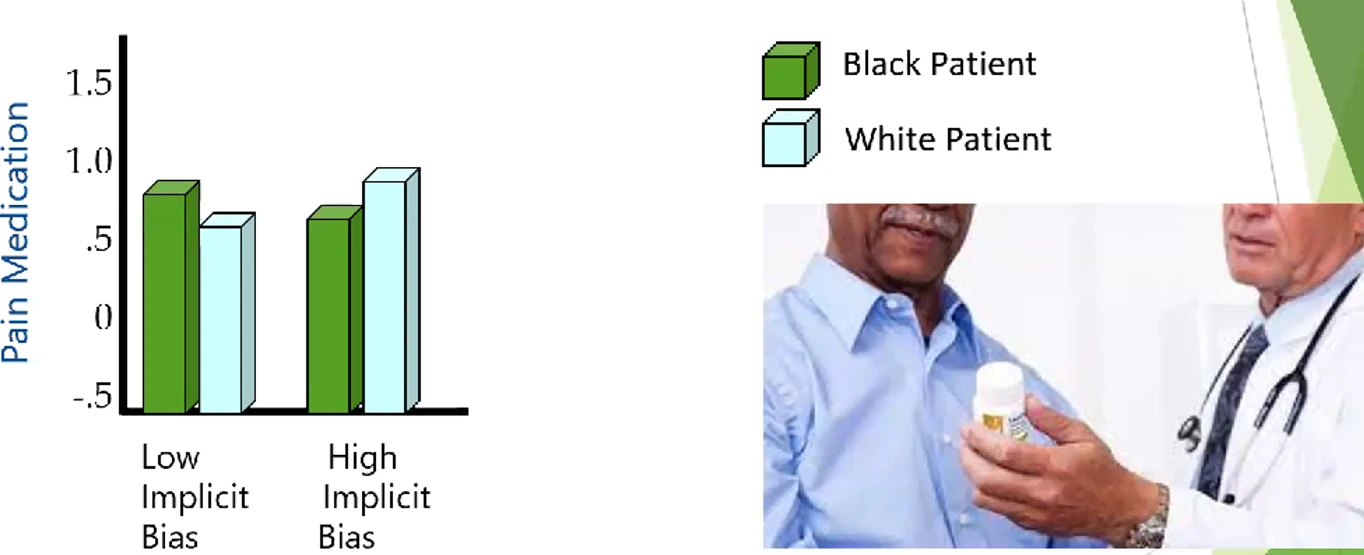
The Impact of Implicit Bias on Medical Decisions: Example of Racial Bias in Pain Care
One area where implicit bias becomes particularly evident is in the treatment of pain. Studies have revealed that healthcare professionals, influenced by stereotypes and ambiguity, may exhibit racial bias in pain care. In the United States, there is a stereotype that Black individuals experience less pain than White individuals, which can result in undertreatment. Additionally, stereotypes associating Black individuals with criminality and drug-seeking behavior can lead to the withholding of pain medication (Fiscella et al., 2021), which can have detrimental consequences for Black individuals. Ultimately, this perpetuates racial disparities in healthcare.
Implications for Patient Interactions and Outcomes
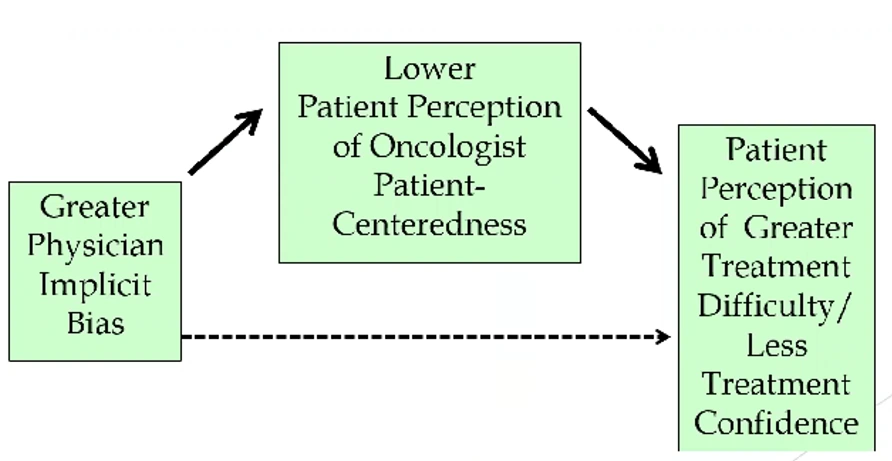
Implicit bias among healthcare providers can also affect patient interactions and outcomes, thereby leading to racial disparities in healthcare. Studies have found that providers with higher levels of implicit bias exhibit shorter visits, faster speech, less patient-centeredness, and reduced supportiveness during interactions with Black patients (Fiscella et al., 2021). Patients, in turn, perceive these behaviors and report feeling less involved, respected, and trusting of their healthcare providers. This lack of trust can negatively impact treatment adherence and patient outcomes, particularly in critical areas such as cancer treatment (Epstein, 2005).
Inequalities in medical settings due to biases in Norway
“Despite Norway’s longstanding efforts to reduce inequities through welfare policies and structural measures, inequalities in health and social determinants of health persist and, in some groups, are widening” (Goldblatt et al., 2023). Dr. Dovidio explained that implicit bias, particularly among healthcare providers, plays a significant role in perpetuating these racial disparities in healthcare. Even in a perfect medical system, biased doctors can lead to biased health outcomes. According to Dr. Dovidio, to achieve true equity, it is crucial to address both social inequities and the biases present in healthcare professionals. Dr. Dovidio explored the impact of implicit organizational bias, highlighted strategies to mitigate bias, and emphasized the importance of addressing racial bias in medical practice.
Implicit Organizational Bias
Next, Dr. Dovidio introduced the concept of implicit organizational bias which refers to how biases become ingrained within the hidden norms and functions of organizations, influencing staff perceptions and behaviors in biased ways (Desai et al., 2021). Organizations operate as organisms with their own goals, motivations, and communication mechanisms. They can perpetuate biases by reflecting societal biases and reinforcing individual biases. Bureaucratic centering, driven by the goal of efficiency, often leads to biased treatment: Healthcare organizations tend to prioritize patients who are healthy, wealthy, and White, neglecting those who require more time and tend to be members of underrepresented groups.
Addressing Racial Disparities in Healthcare
According to Dr. Dovidio, interventions must target individuals, interpersonal dynamics, and organizational structures to combat racial bias in medicine. Diversity education alone has limited effectiveness in reducing bias. Observing bias among professors, instructors, and medical staff can increase implicit bias among doctors in training. On the other hand, intergroup contact, or meaningful experiences with members of other racial groups, can significantly reduce implicit bias. Providing experiential learning opportunities that challenge existing associations and foster positive interactions is crucial in overcoming biases.
Addressing Racial Bias in Medicine: On the Same Team
Changing the structure and environment within healthcare settings can profoundly reduce bias and subsequently racial disparities in healthcare. In one study by Dr. Dovidio and colleagues, a clinic divided into different wings, with one emphasizing that doctors and patients were on the same team, yielded significant results. The wing that promoted a sense of shared responsibility, joint decision-making, and cooperation between doctors and patients fostered trust and patient-centered care. Color-coding rooms, buttons, and pens to reinforce the concept of being on the same team further enhanced the positive outcomes. By creating a bond that transcends racial differences and focuses on shared goals, healthcare providers can overcome implicit biases and improve patient outcomes.
Conclusion
Reducing implicit bias in mental healthcare is essential to guarantee equality and fight racial disparities in healthcare. This requires a comprehensive approach that addresses individual, interpersonal, organizational, and structural factors. It is crucial to recognize the joint influence of these factors and implement strategies that challenge biases at all levels. Healthcare professionals can provide more equitable care by acknowledging and confronting implicit biases. Additionally, organizations must create inclusive environments, support ongoing education and reflection, and prioritize patient advocacy and representation. By working collectively and continuously striving for improvement, we can make significant progress in addressing implicit bias and achieving equitable mental healthcare for all individuals regardless of their skin color or cultural background.

Literature
Alegría, M., Chatterji, P., Wells, K., Cao, Z., Chen, C. N., Takeuchi, D., … & Meng, X. L. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric services, 59(11), 1264-1272. https://doi.org/10.1176/ps.2008.59.11.1264
Desai, M. U., Paranamana, N., Restrepo-Toro, M., O’Connell, M., Davidson, L., & Stanhope, V. (2021). Implicit organizational bias: Mental health treatment culture and norms as barriers to engaging with diversity. American Psychologist, 76(1), 78. https://doi.org/10.1037/amp0000621
Epstein, R. M., Franks, P., Fiscella, K., Shields, C. G., Meldrum, S. C., Kravitz, R. L., & Duberstein, P. R. (2005). Measuring patient-centered communication in patient–physician consultations: theoretical and practical issues. Social science & medicine, 61(7), 1516-1528. https://doi.org/10.1016/j.socscimed.2005.02.001
Fiscella, K., Epstein, R. M., Griggs, J. J., Marshall, M. M., & Shields, C. G. (2021). Is physician implicit bias associated with differences in care by patient race for metastatic cancer-related pain?. PLoS One, 16(10), e0257794. https://doi.org/10.1371/journal.pone.0257794
Goldblatt, P., Castedo, A., Allen, J., Lionello, L., Bell, R., Marmot, M., … & Ness, O. (2023). Rapid review of inequalities in health and wellbeing in Norway since 2014. Institute of Health Equity. https://www.instituteofhealthequity.org/resources-reports/rapid-review-of-inequalities-in-health-and-wellbeing-in-norway-since-2014
Green, T. L., Vu, H., Swan, L. E., Luo, D., Hickman, E., Plaisime, M., & Hagiwara, N. (2023). Implicit and explicit racial prejudice among medical professionals: updated estimates from a population-based study. The Lancet Regional Health–Americas, 21. https://doi.org/10.1016/j.lana.2023.100489
Hahm, H. C., Cook, B. L., Ault-Brutus, A., & Alegría, M. (2015). Intersection of race-ethnicity and gender in depression care: screening, access, and minimally adequate treatment. Psychiatric Services, 66(3), 258-264. https://doi.org/10.1176/appi.ps.201400116
Tajfel, H., & Turner, J. C. (1986). The Social Identity Theory of Intergroup Behavior. İçinde Worchel, S. & Austin, WG (Eds.), psychology of ıntergroup relation (ss. 7-24). https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=1584694



